Every year, over 115 million units of blood are donated worldwide; this is especially critical because for patients who need a blood transfusion, there are no alternatives. In fact, in the US, upwards of 70% of the population will receive a blood donation at some point in their lives.
Check out the Answers to Common Blood Donation Questions
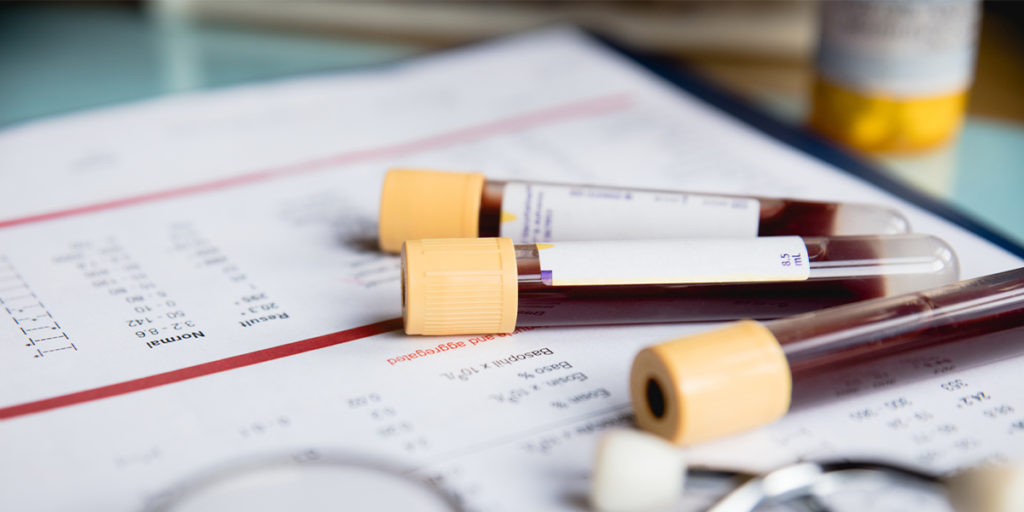
Advancements in blood donor screening and testing to ensure a safe blood supply have been influential in lowering the risk for some transfusion-transmitted infections due to infectious pathogens including viruses, bacteria, and parasites. However, data has shown that reactive screening tests do not eliminate transfusion-transmitted infection due to previously unrecognized pathogens (the Zika virus was a notorious example of this). This is because there is often a delay between the identification of a new pathogen, understanding the risk of transmission by blood, and the development of a blood donor screening test.
What is the Solution?
Recognized as an effective measure for reducing transfusion-transmitted infectious (TTI) risk, pathogen reduction for platelet components provides a holistic solution to blood center and hospital clients alike, ultimately benefiting patients who need it most. Additionally, pathogen reduction complies with the FDA’s guidance on addressing bacterial contamination and it reduces risk beyond bacteria with mitigation of TTI due to viruses and parasites, as well as TA-GVHD due to T-Cells. Additionally, platelets and plasma do not require replication of DNA nor RNA to deliver therapeutic benefit, so targeted inactivation of pathogen DNA and RNA leaves the components of the donated blood functional and minimizes the risk of TTI.
The goal of pathogen reduction technology—note that this is a technology, as opposed to a test—was to create a process for blood banks to treat blood components with a single procedure. This streamlines operations: pathogen reduction is an alternative to bacterial testing, CMV testing, and gamma irradiation: in other words, one technology becomes a suitable replacement for three time-consuming tests. Because when we consider the blood shortage on both national and local levels, making as much blood available for when it’s needed can literally make the difference between life and death.
Pathogen reduction technology mitigates the need for extensive testing.
How Does it Work?
At South Bend Medical Foundation, we turn to the INTERCEPT Blood System. This solution uses amotosalen (a psoralen) and UVA light to cross-link nucleic acids, thereby inactivating a broad range of viruses and bacteria. After we process the platelets, residual amotosalen is removed and the platelet product has normal functional and storage characteristics, reducing the risk of transfusion of pathogens.
What does the Future Hold for Blood Supply Safety?
Well, with multiple new emerging infectious microbial pathogens being recognized as potential threats, some people unknowingly infected with these diseases will then become blood donors, resulting in possible transfusion-transmitted infection. The result is an unintentional spread of yellow fever and the previously mentioned Zika virus. Pathogen inactivation technology is now used in many countries for the preparation of platelet and plasma components. As of 2020, more than seven million blood components treated with this technology have been transfused, and in some countries, it has become the standard of care. And with the emergence of the COVID-19 virus, there is an increased interest and need for blood centers to prepare for any future pandemics.